Health In Rhyme
If you’re not reading Ross’s daily health updates in rhyme , you’re really missing out.
Comments Off on Health In Rhyme

If you’re not reading Ross’s daily health updates in rhyme , you’re really missing out.
Comments Off on Health In Rhyme
I was going to be sarcastic and snarky and critical in an attempt to be funny, but I don’t think it’d work.
These elementary school drawings of human anatomy are surprisingly good. You’ve got muscles attached to bones, a simplified arterial and venous circulation (the renal veins are in front of the arteries, Sarah, and I hope that’s not blood in the ureters), and a nice little kidney (renal pelvis is a bit off).
Okay, so I was still critical. I’m sure they’re better than I could’ve done at their age.
Not much worse than the first year medical students!
A short-but-excellent piece on NPR discusses the trend of medical students changing their preferences for specialties . It’s worth the 8 minutes.
I think the piece is right–my generation has very different priorities than my parents’ generation. While we’re just as hard-working and driven, we want to have a more of a life. We want balance. Or maybe we just want it all–seeing patients, of course–but also families, social lives, and hobbies. I also think it’s unfortunate–and dangerous–to be pumping out such a small number of primary care doctors. But we clearly reward specialists with higher pay and, in many cases, better “hours.” We’re in big trouble in 20-30 years, when the millions of baby boomers need primary care, but all we’ve got is specialists.
I believe I’m ultimately very priveleged to be granted the opportunity to pursue a career in medicine–to receive more education than 99% of the rest of the world–and along with that comes a responsibility. Sacrifice. But ultimately, I want what everyone else wants: time to spend with my family and friends, and time to do the things I enjoy. We’re so focused on the scientific and causational in medical school that religion seems further and further from the truth; if we really only get one turn in this thing called life, I don’t want to miss out on it all. As always, it’s finding the balance that’s the key.
Kevin, M.D. is hosting the third Grand Rounds. Go check it out!
Comments Off on Grand Rounds 3
 It’s
National Coming Out Day today
, and in celebration I thought I’d post some tips and guidelines on how to make yours a LGBT-friendly practice, since the AMA believes that “the
physician’s nonjudgmental recognition of sexual orientation and behavior enhances the ability to render optimal patient care in health as well as in
illness.” (Note: most of these tips are taken from
The ABCs of Sexual Health
, in the BMJ, and
Creating a Safe Clinical Environment for Lesbian, Gay, Bisexual, Transgender and Intersex (LGBTI) Patients
, an excellent guide (pdf) free from
GLMA
.) These are not monumental, folks. It’s the little stuff that counts. Trust me.
It’s
National Coming Out Day today
, and in celebration I thought I’d post some tips and guidelines on how to make yours a LGBT-friendly practice, since the AMA believes that “the
physician’s nonjudgmental recognition of sexual orientation and behavior enhances the ability to render optimal patient care in health as well as in
illness.” (Note: most of these tips are taken from
The ABCs of Sexual Health
, in the BMJ, and
Creating a Safe Clinical Environment for Lesbian, Gay, Bisexual, Transgender and Intersex (LGBTI) Patients
, an excellent guide (pdf) free from
GLMA
.) These are not monumental, folks. It’s the little stuff that counts. Trust me.
Above all, listen, don’t make assumptions, and always be respectful.
Creating a Welcoming Environment:
On Interviewing:
On Counseling:
If you have questions or comments, please post them here; it’d be great to have an open forum to figure these issues out if you’re unsure about them.
Update: Two more great resources from AMSA : Do Ask, Do Tell , and the June 2001 issues of the AJPH .
A recent Ask Metafilter thread has given me pause lately, partially because of my own involvement, and partially because of the outcome.
headspace posts this as her question:
You Are Not A Doctor: Three weeks ago, I got a nasty head cold that never quite went away. It’s now settled into my chest, and I have a chronic, slightly productive cough. Ordinarily, I would just wait it out, but I’m exhausted, can’t really get a full breath, and the stuff I’m coughing up tastes like bleach. I swear, I haven’t been inhaling or gargling bleach. I do have an appointment to see my doctor on Wednesday (the earliest I could get in,) but I was wondering if anyone else had had these symptoms and could tell me what caused them, so I can quit Googling medical conditions and diagnosing myself with lung abscesses and tuberculosis.
I hesitate to answer at first–I’m just a medical student, don’t know a whole, could be wrong and lead someone in the wrong direction–but I figure some information is better than none, and as long as I’m not definitive and make clear that I’m just a student, it should be okay. Having just finished pneumonias and respiratory infections, I remember that foul-smelling sputum is a sign of an anaerobic, gram-negative infection. The shortness of breath thing is concerning, but I don’t feel comfortable calling it a pneumonia. (“Can you still be walking around and be as sick as pneumonia?” I ask myself. All the pneumonia cases in class…people were really sick!) So, I post.
Later in the thread, a real live doctor posts in follow-up saying that I’m a bit off–he thinks it’s a fairly serious pneumonia, and that headspace needs to get to an ER before going septic (ie: get bacteria in your blood, and get really, really sick as your body freaks out in response). I feel a bit chided–this is the perfectionist in me–but it’s something I’ve got to get used to. I’m new at this, I don’t have experience, I don’t know all the answers, I’m learning. I will be wrong again. (This further makes me wonder if I should have posted in the first place.) I do , however, come away with a better understanding of mycoplasma pneumonia , also known as “walking pneumonia.”)
The whole post brings up issues of online diagnosing and malpractice that make me uncomfortable. Is it unethical to try to diagnose in the dark without all the data? Without actually seeing–that is, observing–the patient? Or is it unethical not to try to provide a diagnosis, or at least a recommendation that the patient go to their doctor or the ER? In this case, no one knew headspace’s age, exposure history, history of present illness, past medical history, social history, family history, sexual history.
But the more disturbing question, for me at least, comes from headspace’s follow-up :
Well, gram gets points for the diagnosis- I have bronchitis, and lots of lovely antibiotics and codeine cough syrup now, but ikkyu gets points for sending me to the doctor today. If I’d waited ’til Wednesday and felt any better, I probably wouldn’t have gotten the chest X-ray to rule out pneumonia, and they wouldn’t have found the mass that’s in my right lung. I’m a little shell-shocked, but better to find out now than when it’s too late.Thank you guys all for your good wishes and your suggestions, I really appreciate it.
It’s these freaky “what ifs” that have always bothered me. What if the doctor didn’t say headspace should have gone to the ER? What if she just took my advice, didn’t get the chest x-ray, and didn’t find out about the right lung mass until later? Is there something more to this than mere coincidence? Fate? Destiny? “Everything happens for a reason?” Or is this just random chance? The spiritual side of me prefers the former, while the medical side argues for the latter.
Been wanting to post this for weeks, but as I’m feeling just crappy enough to justify not studying, now’s the perfect time.
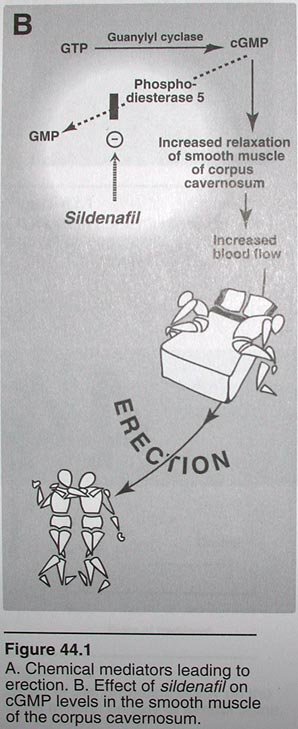
I use Lippincott’s Illustratred Pharmacology for a study tool-it’s an excellent book, and really well organized. I was flipping through the pages a couple weeks ago and came across sildenafil-ie: Viagra -and found what is, quite possibly, the best illustration of a drug mechanism ever :
Yes, that’s right. Eat too much black licorice, and your heart can stop.
(Okay, okay, it’s a bit of a dramatic extreme, but it’s true. I swear .)
Black licorice contains a compound called glycyrrhizic acid, which mimics a hormone in your body (aldosterone), which causes you to lose potassium through your urine. This causes what’s called hypokalemia , which can lead to abnormal heart rhythms. (Maintaining the right level of potassium in your body is vitally important. Too much or too little can cause abnormal heart rhythms. Luckily your kidneys usually keep everything juuuuust right.)
Just added a couple new medbloggers to the list : Medical Mad House and a The Examining Room of Dr. Charles . Welcome, guys!
We went to a nursing home today to practice our history and physical exam skills today, and then presented to our preceptor (again, another awesome name: Dr. Pompei). We then went back to several patients to listen and observe some interesting findings–a heart murmur, a gigantically swollen leg, and lastly, a very soft murmur in a patient recovering from a hip replacement.
Sharing the room with the hip replacement patient was an elderly gentleman, dying of cancer. He drew much more attention than the heart murmur. His muscles were wasting away, his face was thin, and only his eyes and head moved around the room, the rest of his body remaning still. I felt intensely uncomfortable, but still wanted to make some sort of effort to try to connect. I was extremely judgmental of everything I said:
* “How are you doing, sir?” (How do you
think
he’s doing, Graham? He’s dying, you idiot.)
* “Can I get you anything?” (What could you get him? Dr. Pompei just asked him the same thing 2 minutes ago.)
And then a couple minutes of awkward silence before I said goodbye.
I guess I just wanted to fill some sort of loneliness void for him, even if it was just for a couple minutes. But I think that it was a silly assumption a) that I could even accomplish that b) that he even wanted that or c) that a 2 minute conversation could even do that.
My experience is colored by my grandmother’s death in a nursing home when I was thirteen. She died of ALS/Lou Gherig’s Disease , and I can’t help but think how very selfish I was at that age–wanting to play computer games or watch television than be stuck visiting her for an hour. My visit was also colored by the fact that a woman was playing piano by ear at the nursing home, just as my own grandmother used to do.
If a large proportion of medical care is so routine: sore throats, ear infections, colds and flus–maybe we should make room for physicians to take on a higher calling: helping people maximize their number of years of high-quality life, and then helping them to die with dignity, respect, comfort, and peace.