(If you’re just joining us,
here’s the introduction
.)

People die.
I wish it wasn’t so.
 Over the next 30 years, America is going to be seeing its population growing in the older age groups more than the younger ones. We will see a massive increase in our
elderly population, who tend to be sicker, have more chronic diseases complicating their care, and have weaker immune systems, making them more likely to get sick
with an infection in the first place. And as people will be living longer, they will have increased years for possible health expenditures, including medical
interventions that may or may not be necessary.
Over the next 30 years, America is going to be seeing its population growing in the older age groups more than the younger ones. We will see a massive increase in our
elderly population, who tend to be sicker, have more chronic diseases complicating their care, and have weaker immune systems, making them more likely to get sick
with an infection in the first place. And as people will be living longer, they will have increased years for possible health expenditures, including medical
interventions that may or may not be necessary.
At present, our health care system already appears to be unable to handle this load of patients. It will not improve with a higher quantity of patients. While we can
certainly build more beds and more hospitals, we run into a more serious supply problem: doctors and nurses to staff them. (Taking Jack Wennberg’s
Dartmouth Atlas of Health Care
only complicated the issue further, showing that less health care = healther patients, that there are huge regional variations in care patterns with little change in
outcomes by region, and that
30% of Medicare’s budget is spent on the last year of someone’s life
.)
 We also currently have a system where, due to legal fears (and the fact that Medicare will pay for it), doctors and hospitals end up providing ultimately futile care
(ie: using health care resources that will not ever be able to meet the goals of care for a patient) due to either a) lack of an advance directive stating the
patient’s wishes, b) family disagreement over the patient’s wishes, with threats of a lawsuit, and c) no standard by which to determine how to proceed in
these situations. This is often ultimately bad for the patient, and is certainly not without harm: all interventions carry risk, and most cause at least some degree
of pain or discomfort. Add in the oft-quoted Hospice statistic that while 90% of patients, when asked, want to die at home, 90% currently die out-of-home.
We also currently have a system where, due to legal fears (and the fact that Medicare will pay for it), doctors and hospitals end up providing ultimately futile care
(ie: using health care resources that will not ever be able to meet the goals of care for a patient) due to either a) lack of an advance directive stating the
patient’s wishes, b) family disagreement over the patient’s wishes, with threats of a lawsuit, and c) no standard by which to determine how to proceed in
these situations. This is often ultimately bad for the patient, and is certainly not without harm: all interventions carry risk, and most cause at least some degree
of pain or discomfort. Add in the oft-quoted Hospice statistic that while 90% of patients, when asked, want to die at home, 90% currently die out-of-home.

I’m certainly not ready to say that “at age 80, you get no more health care, and if you die, you die” as some have proposed. If you spend even a day
in a hospital or medical clinic you see the broad, broad variation of what 80 means. 80 can be fully, 100% functional, with energy and vibrance of a 25 year-old; 80
can mean severe, advanced Alzheimer’s with 3 heart attacks and the inability to dress or feed oneself.
What we need is a better prognosticator. Some way to figure out when a person’s last year of life will be. (I worry this may never come; we humans are just too
damn unique, complex, and confusing, and the awesome human spirit often beats the actuarial tables in the betting game.)
In one corner, we have the elderly patient. He doesn’t want, in general, to die in a hospial, connected to ICU tubes, fingers and tubes in every orifice. It is
not a dignified death. In fact, in retrospect, when most people finally learn about and enroll in hospice, their reaction is “I wish we would have known about
this sooner.” In the other corner, we have the health care system, which can’t figure out how to balance the needs of society. So what do we do? We do
what any American would do: we offer choice.
Experiment: we offer people, say, 90 and above $30,000 and 100% free hospice care. In exchange, they agree to seek simple or comfort care only. See, those “last
6 months” costs or “last 1 year” costs are worth real, American dollars. And my guess is if you ask these people what they want with their final
time, it’s not to spend it in a hospital or a doctor’s office. Maybe it’s to see Italy or France. Or to take a vacation with their
great-grandchildren to Disneyworld. Or buy a fast car. Or invest it in the stock market. Who knows? I certainly don’t pretend to know what you want.
Again, this would not be a Draconian requirement, merely an option. If you’re going to be spending your hard-earned insurance dollars on something, perhaps you
should get a choice–hospital food and IV sticks daily, or Paris? Sure, maybe you die a little sooner because you’re not seeing every doctor every month,
but we certainly allow people to die sooner by smoking cigarettes or ride a bike without a helmet, right?
Even if this isn’t the option you choose, I strongly believe that Hospice should be free. Not only because it’s a simple, humane, dignified,
cost-effective way to provide closure to people’s lives, but that it is what most people want at the end of life. It makes people comfortable and addresses
their symptoms while giving them the needed medical follow-up to meet the goals they want for their short time remaining: often peace, closure, and time with the ones
they love.
Second, I believe everyone with Medicare (or perhaps everyone with insurance, or everyone admitted to the hospital?)
must
have an advance directive. Even if it’s “I want everything done,” everyone must have
something
. Say we tell everyone they must have one by 2010, and if they have one by 2009, they get an extra $200 tax credit (first carrot, then stick). There are too many
people who ignore the fact that they will die (see above: everyone does) and it causes problems for the entire society. (Remember, we’re all in this together.)
From the family members it tears apart to the doctors and nurses who feel they are providing futile care, to your loved one who needs a hospital bed but cannot get
one because the hospital is full.
I believe we are truly disrespecting and taking the dignity from our loved ones by not knowing what they would want. We owe it to our parents, spouses, and loved
ones to be able to represent them and their wishes correctly.
We’ve now had ventilators and life support systems for what, 50 years? — but we still can’t seem to face up to the fact that many of our loved ones
will spend time incapacitated at some point in their lives and we should know what to do when they are.
Third, we must recognize that often, family bickering about what a parent or other loved one “would have wanted” is not truly bickering, but more often a
stage in the grief process — denial (“Mom is not going to die, do everything!”), anger (“How *dare* you say that mom is dying! Do
everything!”) or bargaining (“Can we just try chemotherapy for two more weeks? Do everything!”). If we understand them from this perspective, it may
be easier to resolve these issues.
Note: I toyed with the idea of “cost-sharing” for futile care, but I believe this to be a cruel way of enforcing policy–that “mom is going to
die because I can’t afford to pay for her care.” I’d much rather setup a system that makes it “okay” for mom to die than
“forcing” her to die. (See my upcoming post on Patient Autonomy.)
Finally, language affects the way we understand our world. I wholely support the efforts to change terms “do not resuscitate” to “allow natural
death,” and “life support” to “artificial organ support,” as often our tools are merely preserving organs, not a patient’s life.
As Reverend Chuck Meyer
discusses the former terms
:
An order to Allow Natural Death is meant to ensure that only comfort measures are provided. By using the AND, physicians and other medical professionals would be
acknowledging that the person is dying and that everything that is being done for the patient–including the withdrawal of nutrition and hydration–will
allow the dying process to occur as comfortably as possible. While a DNR patient in Intensive Care might be put on a ventilator, given artificial hydration, or have
a feeding tube inserted, an AND patient would have all of those things withdrawn, discontinued, or not even started, since such treatments are painful and
burdensome for the terminally ill. The AND would prevent this unintentional pain and simply Allow a Natural Death.
(
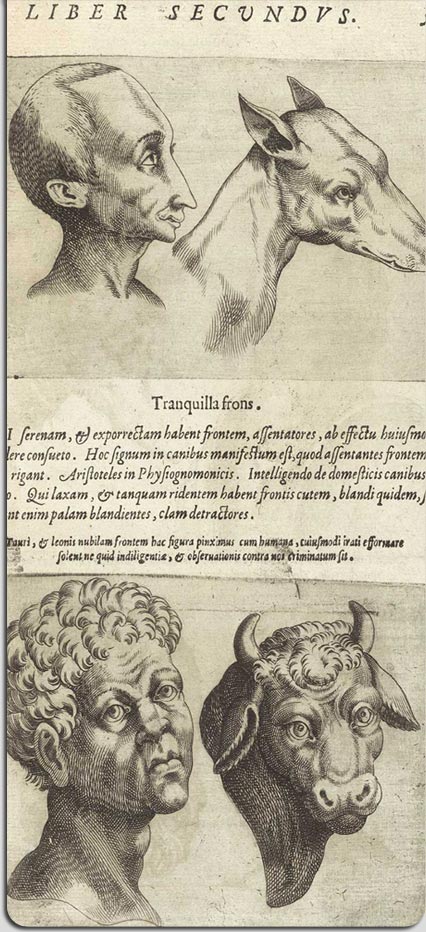
Image Creative Commons licensed at Flickr.
)
19 Comments »




 Over the next 30 years, America is going to be seeing its population growing in the older age groups more than the younger ones. We will see a massive increase in our
elderly population, who tend to be sicker, have more chronic diseases complicating their care, and have weaker immune systems, making them more likely to get sick
with an infection in the first place. And as people will be living longer, they will have increased years for possible health expenditures, including medical
interventions that may or may not be necessary.
Over the next 30 years, America is going to be seeing its population growing in the older age groups more than the younger ones. We will see a massive increase in our
elderly population, who tend to be sicker, have more chronic diseases complicating their care, and have weaker immune systems, making them more likely to get sick
with an infection in the first place. And as people will be living longer, they will have increased years for possible health expenditures, including medical
interventions that may or may not be necessary.
 We also currently have a system where, due to legal fears (and the fact that Medicare will pay for it), doctors and hospitals end up providing ultimately futile care
(ie: using health care resources that will not ever be able to meet the goals of care for a patient) due to either a) lack of an advance directive stating the
patient’s wishes, b) family disagreement over the patient’s wishes, with threats of a lawsuit, and c) no standard by which to determine how to proceed in
these situations. This is often ultimately bad for the patient, and is certainly not without harm: all interventions carry risk, and most cause at least some degree
of pain or discomfort. Add in the oft-quoted Hospice statistic that while 90% of patients, when asked, want to die at home, 90% currently die out-of-home.
We also currently have a system where, due to legal fears (and the fact that Medicare will pay for it), doctors and hospitals end up providing ultimately futile care
(ie: using health care resources that will not ever be able to meet the goals of care for a patient) due to either a) lack of an advance directive stating the
patient’s wishes, b) family disagreement over the patient’s wishes, with threats of a lawsuit, and c) no standard by which to determine how to proceed in
these situations. This is often ultimately bad for the patient, and is certainly not without harm: all interventions carry risk, and most cause at least some degree
of pain or discomfort. Add in the oft-quoted Hospice statistic that while 90% of patients, when asked, want to die at home, 90% currently die out-of-home.
